Hot Flashes, Why? Welcome to the World of Hormones
Hormone replacement therapy (HRT) for women has long been disregarded, demonized, and feared to the extent that hormones are almost never looked at or considered in any aspect of health with a routine check-up. Wouldn’t you be curious to find out what’s going on in one of the most important systems in your body? The endocrine system is one of the most crucial aspects of health, especially mental health, that is often an afterthought. Feeling like you’re tired? Maybe you have low libido (sex drive), feeling down or depressed, lack confidence, sky-high anxiety, or hot flashes that won’t stop. A woman’s body is like a highly tuned Formula 1 car. It takes premium fuel and needs a deep understanding. So, if you’d like to find out why your engine keeps overheating, providing you with hot flashes and abnormal feelings that are hard to explain, this is the article for you.
What are hormones and what you need to know
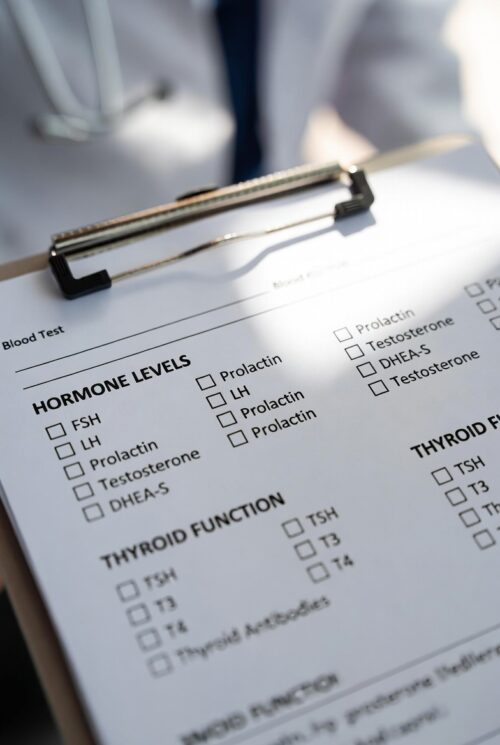
Hormones are little messengers in your body that regulate a multitude of things. A cascade of signals produced by endocrine glands or specialized cells that travel through the bloodstream, managing mood, growth, metabolism, reproduction, vitality, stress response, and sleep. These are just a few, and only surface level, of what these chemical messengers do to coordinate the body’s activity to maintain balance (homeostasis). And if you have never had a hormone panel done, along with a complete metabolic panel (CMP), there is no telling what might be running smoothly, or breaking down in your fine-tuned racing machine.
Let’s Start with Estrogen
The primary female hormone. Estrogen is actually three hormones: estradiol (E2), estrone (E1), and estriol (E3). Estradiol is the most potent and important. Let’s look at estradiol in a breakdown of the body’s systems.
Reproductive System:
- Develops breasts, hips, and female body shape
- Thickens the uterine lining for pregnancy
- Regulates the menstrual cycle
- Keeps vaginal tissue healthy
Bones:
- Keeps bones strong by slowing down breakdown
- Why postmenopausal women have a higher osteoporosis risk than men.
Brain:
- Affects mood and memory
- Influences serotonin production, “the feel good” hormone. (mood, sleep, memory)
Heart & Blood:
- Helps keep blood vessels flexible. (Prevents atherosclerosis and inflammation in vessels)
- Affects cholesterol, inhibits plaque build-up up and oxidation of cholesterol particles.
Skin:
- Maintains collagen and moisture – prevents skin loosening and wrinkles
- Affects skin thickness – supple and plump skin
Estrogens Role in Bone Density and Osteoporosis
Women lose 20% of bone density after 5-7 years after menopause. Post-menopausal women are roughly 4x more likely to develop osteoporosis than men of the same age. The estrogen crash at menopause is the single biggest risk factor for bone loss in humans. Why? Well, estrogen inhibits osteoclast activity (the cells that break down bone). And allows for osteoblasts to catch up. Think of the osteoblasts as the construction crew (blasts build), and osteoclasts (clasts consume) as the demolition team. When estrogen drops, the demo team (osteoclasts) goes wild. Bone breakdown increases dramatically, and the construction crew (osteoblasts) can’t keep up. You need both for healthy bones. Think out with the old, in with the new.
What Happens when Women Lack Estrogen?
The lack of estrogen throws off homeostasis (balance), and the bone density is severely affected. Hip fracture is a real concern with everyone, but especially for women. Globally, hip fracture rates are about 2 times higher in women than in men, with 72% of cases in women. And after the fracture, we see up to a 23% increase in mortality rate 90 days post incident. What we’re getting at here is that estrogen is extremely important in women. And you should be getting labs done to test the levels. It’s measured in picograms per milliliter (pg/mL), and you have to look at estradiol. If the doc ordered total estrogens, your not getting the accurate picture.
So should all women be on estrogen after menopause? Not nessecairly. It is your choice, and with ANYTHING you take, to include the prescriptions that come from the doctor, there is a level of risk. But HRT got a bad rap over the last few decades, and here’s why.
The Dogma of Hormone Replacement Therapy in Women
The reputation of hormone replacement therapy (HRT) was significantly damaged by the 2002 Women’s Health Initiative (WHI) study, which examined the effects of a specific hormone therapy drug. This drug contains conjugated equine estrogens , or pregnant mare urine, yikes. Media coverage of the results was dramatic, leading to widespread public panic and a sharp drop in HRT prescriptions. The initial reporting oversimplified the findings, suggesting that all forms of HRT were dangerous for all women. Highlighting the potential for breast cancer from HRT, there was less than a percent (0.8%) occurrence of it happening. It was blown out of proportion by the media, and then the dogma stuck.
We now use bio-identical hormones. A version that is essentially the same as what your body produces. Not a squirt of tinkle from a pregnant horse. All this to say, you should absolutely speak to an informed medical professional on the topic of HRT before beginning. They should be doing a panel, physical examination, and general health overview.
Alright, so now that the fear of HRT has been debunked and we’ve done a disservice to millions of women over the last 2 decades, let’s look at the hormones you should be looking into alongside estrogen. Because if the Doc just gave you estrogen pills, there might be more to it. Remember, this is about empowerment through info, not DIY prescribing.
What Other Hormones to Look at Other than Estrogen?
Pregnenolone
“The Mother of hormones.” This one’s the precursor to nearly all your steroid hormones, including progesterone and DHEA, and levels drop sharply in perimenopause, fueling brain fog, anxiety, and sleep issues. Emerging research positions it as a neurosteroid hero for menopausal depression. A clinical trial is underway testing it specifically for mood lifts in women, with early data showing it calms overactive stress responses without the sedation of typical antidepressants. Another study highlights its role in skin health and neurological protection, making it a smart add-on if estrogen alone leaves you feeling wired but wiped. Aim to check serum levels. Below 50 ng/dL, could explain why your HRT feels incomplete.
Progesterone
The yin to estrogen’s yang, countering breast tenderness, heavy moods, and endometrial risks. Meta-analyses confirm that adding micronized progesterone to HRT slashes insulin resistance (better blood sugar control) and even sharpens verbal memory in midlife women, without the clot worries tied to synthetic versions. It’s a game-changer for sleep too, as levels crash post-ovulation in menopause. Studies show it shortens time to fall asleep, stretches sleep duration, and cuts wake-ups from hot flashes or sweats, which plague up to 80% of menopausal women.
With progesterone’s knack for boosting GABA, the neurotransmitter that quiets racing thoughts, it promotes that “ahh, finally” relaxation. Low progesterone links to insomnia and mood dips. Sleep is extremely important and often overlooked. Restoring progesterone and improving sleep could massively turn your life around. Opt for bio-identical oral progesterone for that sleep-specific punch. Topicals or synthetics skip the full GABA boost. Chat with your doc about dosing (often 100-200 mg nightly), and track how it vibes with your cortisol rhythm via a simple saliva test. (A “Dutch Test” is a good place to start)
If yours is under 1 ng/mL in the luteal phase (or undetectable post-menopause), pushing for bioidentical forms could round out your protocol nicely.
Testosterone
Testosterone is an essential hormone for women, produced primarily in the ovaries and adrenal glands, yet it’s often misunderstood. A key misnomer stems from viewing testosterone as exclusively a “male” hormone, leading many doctors to hesitate in prescribing it for hormone replacement therapy (HRT) in women, especially during perimenopause or menopause. This outdated perspective ignores that women naturally produce testosterone, albeit much less than men, yet still necessary as a vital role in health for women.
Common testosterone myths for women are
It’s only for libido:
While it does enhance sexual desire, testosterone also supports energy, mood, muscle maintenance, and bone health.
It causes masculinization:
At physiological doses (mimicking natural levels), it doesn’t lead to unwanted effects like facial hair or voice deepening. These occur only with supraphysiological (excessive) doses.
Testosterone Truths for Women
A 2024 pilot study on transdermal testosterone in peri and postmenopausal women found significant enhancements in cognitive function, including better memory and executive skills, alongside reduced mood disturbances like irritability and low mood, with participants reporting sharper focus after just 12 weeks. This aligns with broader evidence from a 2025 review in The Pharmaceutical Journal, which highlights testosterone’s contributions to metabolic function, such as improved insulin sensitivity and lipid profiles, potentially lowering cardiovascular risks by reducing inflammation and aiding fat redistribution away from the abdomen.
Benefits of Testosterone in Women
Women often notice a surge in overall vitality, with fatigue lifting as energy levels stabilize, allowing for more consistent daily activity without the midday crashes common in hormone imbalances. Physically, it supports lean muscle maintenance and bone mineral density, countering the sarcopenia and osteoporosis risks that accelerate post-menopause. Even subtle perks emerge, like smoother skin elasticity from collagen support and better sleep quality, which indirectly amplify these gains. These benefits increase when combined with estrogen-progesterone HRT, especially for women under 60, or within a decade of menopause onset.
Testosterone is extremely important as we age for strength and muscle mass. Another point to address, women will not “bulk up” when weight training or when taking testosterone. It’s going to benefit by increasing lean muscle mass for a sculpted appearance. Muscle mass is far too overlooked as we get older, and women especially should be resistant training to combat osteoporosis, sarcopenia, and overall mood. It’s a natural way to relieve depression, anxiety, and boost your endorphins (your body’s built-in pain killers).
Testoserone Ranges in Women:
Reproductive-Age Women (18-45 years): Total testosterone typically ranges from 15 to 70 ng/dL, with free testosterone at 0.3 to 1.9 ng/dL. Levels peak mid-cycle during ovulation, supporting fertility and energy through estrogen-androgen synergy.
Postmenopausal Women: Total drops to 7 to 40 ng/dL, free to 0.1 to 1.0 ng/dL.
A 25-50% decline from ovarian shutdown, often triggering symptoms if below mid-range.
Recommend restoring to physiologic restoration at 80-100 ng/dL total (70-80% for women in their 30s-40s), avoiding anything over 200-300 ng/dL, which exceeds natural maxima and triggers irreversible issues like voice deepening or clitoral enlargement.
There are many choices for testosterone replacement, like pellets, injections, and creams. For women needing a lower dose, the creams may be most convent and beneficial being as the compounded vanishing cream (24 mg/g, 2 clicks twice daily) gives steady, physiological delivery that mimics natural rhythms, avoids liver impacts, and supports benefits like mood and body composition without clot risks. Pellets are convenient to get every 3 or so months, but the downside is that you can not adjust the dosage as needed.
https://pubmed.ncbi.nlm.nih.gov/26358173
Thyroid Stimulating Hormone
The thyroid serves as the body’s master temperature and metabolism regulator. Looking at Thyroid Stimulating Hormone (TSH) is key to deciding if HRT is the route to take. Thyroid function testing forms the cornerstone of a comprehensive HRT evaluation because the thyroid and reproductive hormones are intricately linked.
Estrogen fluctuations in perimenopause can alter thyroid-binding globulin (TBG), potentially shifting free hormone availability and amplifying symptoms like fatigue or weight gain that overlap with menopause.
Routine baseline testing, ideally fasting, morning draws, rules out subclinical hypothyroidism (TSH >4.0 mIU/L with normal T3/T4), which affects up to 10-15% of perimenopausal women and can worsen hot flashes or mood instability if untreated.
So we must also look at T3 and T4, specifically the “Free” unbound versions. In short TSH (thyroid-stimulating hormone), produced by the pituitary gland, acts as the master regulator, signaling the thyroid to produce T4 (thyroxine, the inactive pro-hormone) and T3 (triiodothyronine, the active form).
Chills, can’t lose weight?
Thyroid dips can mimic estrogen lows by slowing everything down, leading to chills, unexplained weight gain, or that constant “cold hands” issue, making it crucial to check those TSH, free T3, and T4 levels for a full picture. Both hyperthyroidism (high T3/T4) and hypothyroidism (low T3/T4) can cause these symptoms of fatigue, weight changes, mood disturbances, insomnia, and hot flashes.
TSH Levels for Women
TSH: Optimal is 1.0-2.5 mlU/ML
Free T4 (thyroxine) : 0.8-1.8 ng/dL
Free T3 (triidothyronine): 2.3-4.2pg/mL
Don’t Fear Hormone Replacement. But Most Importantly, Know what Is going on in Your Body
In summary, hot flashes and chills, weight gain and weight loss, bone density, and vitality are all credited to hormones. And if you don’t get a glimpse into them or overlook how they affect your body, you can really do yourself a disservice. So why not have a bit of knowledge and perspective, decide how you want to optimize your life, and go forward educated? Hormone replacement is not the answer for everyone, but a deep dive into understanding your body is. Don’t run your premium racing machine on wide open without ever looking under the hood.
Blood Panel Audit, for Free
If you’re interested in a comprehensive health review and want to discuss a recent blood panel, contact us here for a free review.
Take your well being into your own hands. Get educated, informed, and know where to start.