The Ultimate Blood Panel for Heart Health: 8 Essential Tests to Detect CVD Risk Early (2025 Guide)
Blood panel for Heart Health
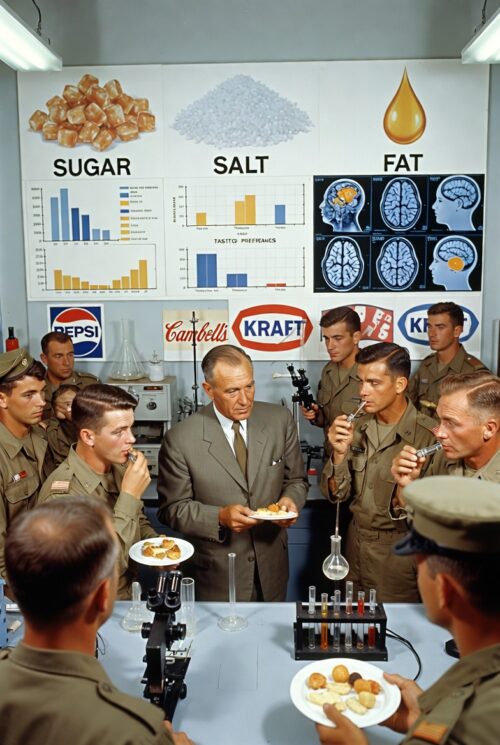
Did you know that in the U.S., someone dies of cardiovascular disease every 34 seconds? A stat straight from the American Heart Association. That is around 2,500 deaths per day in the United States. For years, the health industry has been so focused on cholesterol. Having a high number is bad, and consuming fat is bad. In another blog, we dive into how fat can improve markers and how it helps those with obesity improve arterial health. The issue is not resolving; perhaps it’s time to look at things more closely. Standard cholesterol checks miss the full picture. What if hidden inflammation or genetic ‘sticky’ lipids are silently clogging your arteries? In this guide, we’ll break down 7 powerhouse tests, optimal levels, and actionable steps to optimize health. Ready to take health on as your responsibility?
The 7 Essential Tests in Your Heart Health Blood Panel:
| Test | What It Measures | Why It Matters for CVD Risk | Optimal/Good Levels | Elevated/Bad Levels | Notes |
| Coronary Artery Calcium (CAC) Score | Calcium deposits in coronary arteries via low-dose CT scan; quantifies plaque burden. | Detects early atherosclerosis before symptoms; strong predictor of future heart attacks/strokes. | 0 (no plaque, very low risk <5%). | 100–399: Moderate risk (mild-moderate plaque). >400: High risk (extensive plaque). | Non-invasive; recommended for intermediate-risk adults (e.g., 40-75 years). Age/gender-adjusted percentiles matter too. |
| High-Sensitivity C-Reactive Protein (hs-CRP) | Liver-produced protein marking systemic inflammation. | Chronic inflammation (from high sugar, stress, obesity, etc.) damages arteries and promotes plaque; blood sugar is a top trigger. | <1 mg/L (low risk). | >3 mg/L (high risk). | 1-3 mg/L = average risk. Test twice for accuracy; avoid recent infections. |
| Apolipoprotein B (ApoB) | Number of atherogenic (plaque-causing) lipoprotein particles (e.g., LDL, VLDL). | Better than LDL alone for predicting artery clogging; counts “bad” particles. | <80-90 mg/dL (optimal, especially if high-risk). | >120 mg/dL (high risk). | Often not covered by insurance; part of advanced lipid panel. Lifelong low levels cut heart disease risk significantly. |
| Hemoglobin A1c (HbA1c) | Average blood sugar over 2-3 months (% of red blood cells coated in sugar). | High sugar damages vessels, accelerates plaque, and signals prediabetes/diabetes risk. | <5.7% (normal). | ≥6.5% (diabetes). 5.7-6.4% (prediabetes, increased CVD risk). | Ties directly to CVD; even prediabetes doubles heart event risk. |
| Lipoprotein(a) [Lp(a)] | Genetic lipoprotein similar to LDL but with a “sticky” protein that promotes clotting and plaque. | “Evil twin” of LDL; boosts thrombosis and inflammation risk independently of other lipids. | <30-50 mg/dL (low risk). | >50 mg/dL (elevated; 2-3x higher heart attack/stroke risk). | Mostly genetic (test once); no direct treatments yet, but flags need for aggressive LDL control. |
| Total Triglycerides | Blood fats from excess calories (sugar/carbs turned to fat by liver). | High levels signal insulin resistance; promotes small, dense LDL particles. Alcohol, refined carbs, and oxidized seed oils worsen via inflammation (CRP spike). | <150 mg/dL (normal). | ≥200 mg/dL (high; ≥500 very high, pancreatitis risk). | Fasting test; lowering via diet (low-carb, omega-3s) cuts CVD events by 20–30%. |
| Fasting Insulin | Insulin levels after 8-12 hour fast; gauges cell sensitivity to sugar. | High = insulin resistance (cells “numb” to insulin), leading to high sugar/fats and artery damage. | <8-10 μIU/mL (optimal). | >25 μIU/mL (insulin resistance). | Pairs with HbA1c for metabolic health; under 10 ideal for longevity. |
| Homocysteine | Amino acid byproduct; builds up with B-vitamin deficiencies. | Damages artery linings, promotes clotting/plaque; independent CVD risk factor. | <10-15 μmol/L (normal). | >15-20 μmol/L (elevated; 20-30% higher heart disease risk per 5 μmol/L increase). | Often overlooked; supplement B6/B12/folate if high. Linked to stroke too. |
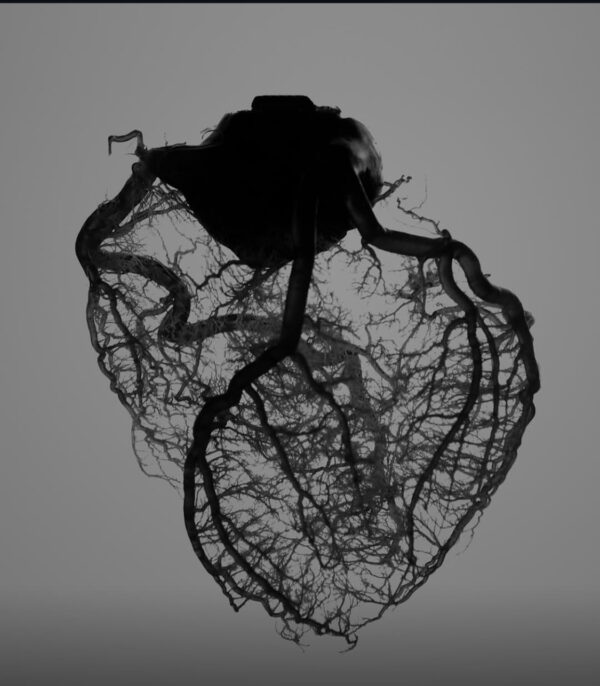
What Is a Coronary Artery Calcium (CAC) Score and Why It’s a Game-Changer for Early Heart Attack Detection?
This non-invasive CT scan measures calcium deposits, a hallmark of atherosclerosis, providing a “plaque burden” number that traditional cholesterol tests often miss.
How It Measures Plaque:
Atherosclerosis (artery hardening) starts with soft, fatty buildup (oxidized cholesterol, macrophages, and Lipoprotein a) that can calcify over time. The CAC quantifies calcium as an “Agatston score” (a number from 0 upward), acting as a proxy for total plaque burden. Zero means clean pipes, higher numbers signal more buildup, even if you feel fine. Sounds easy, right? Unfortunately, insurance and doctors don’t put you in for this until after a heart attack. Times are changing, and updated guidelines are now recommending this for a preventative measure. But medicine guidelines move slowly, especially for the everyday person. PubMed CAC.
Science backs its predictive power. A 2024 meta-analysis of over 100,000 adults under 50 found that a CAC score of 1-100 doubled the risk of cardiovascular events like heart attacks or strokes over 10 years, while scores >400 quadrupled it compared to zero. Another 2024 study in Radiology confirmed CAC=0 signals near-zero risk for major adverse cardiac events (MACE), making it ideal for intermediate-risk folks aged 40–75. See this article here. pubs.cac
To act: If your score is 100+, prioritize nutrition and lifestyle tweaks, start with 30 minutes of daily walking to slow plaque progression. Or exercise “snacks” through the day, ie, 15 air-squats, this is effective for reducing insulin spikes after meals. Check out how high fats can reduce atherosclerosis risk in this recent blog breakdown.
hs-CRP Test Explained: The Fire Alarm for Hidden Artery Inflammation and Heart Disease
hs-CRP is your body’s inflammation smoke detector, produced by the liver. It flares up from culprits like high blood sugar, stress, or belly fat. Signaling chronic fires that erode artery walls and fuel plaque buildup, long before chest pain hits. Recent evidence is compelling. A June 2025 eBioMedicine study of stable coronary patients showed that hs-CRP >3 mg/L independently predicted a 2.5-fold increase in cardiovascular events and all-cause mortality over 5 years. Echoing this, the 2025 ACC Scientific Statement in JACC highlighted a linear hs-CRP-CVD risk link, with levels >2 mg/L raising event odds by 50-100% across broad populations. jacc.org inflammation
Reduce Inflammation:
Cut processed foods, especially those that contain seed oils. Processed Carbs (crackers, bread, chips, cereals) another big one that is causal of inflammation. Reduce these foods and you will have less. Retest in 3 months.
Is LDL the near risk factor? Dive into ApoB:
Standard LDL cholesterol tells you the amount of cholesterol in the blood, ApoB counts the number of carriers needed for those particles in the blood. Why care? More packages equal more chances for them to crash into your artery walls, dump particles, and build plaque (atherosclerosis). It’s sneakier because even if your LDL looks “okay,” a high ApoB count means you’re still at risk, like having a fleet of small, dense particles that slip through cracks more easily.
Heart Connection High ApoB
It is a top predictor of heart attacks and strokes. It’s especially pertinent for folks with diabetes, obesity, or family history, as it flags “particle overload” before symptoms hit.
HbA1c Blood Test: Unmasking Pre-diabetes’ Silent Assault on Your Heart Vessels
HbA1c is a 3-month sugar crust on your red blood cells, revealing average glucose levels that high-sugar/processed food diets scratch into vessel walls, speeding plaque build-up and doubling heart risks, even before full diabetes.
- An April 2024 JAHA cohort of 15,000+ adults linked HbA1c 5.7-6.4% (pre-diabetes) to a 1.5-2x CVD hike, with ≥6.5% tripling events like myocardial infarction or stroke. A May 2025 Diabetology & Metabolic Syndrome meta-analysis echoed this, showing pre-diabetes HbA1c elevates CVD odds by 40% via endothelial damage. Check out the study – AHA Study
Fight Back: If this number is high, reduce carb intake. Time larger meals or meals with cars around workouts, or the most active part of the day. Add in “workout snacks” after meals. 15 air squats, quick walks, especially uphill, or wall sits, which have a litany of benefits (read about them in this blog). There was a great meta-analysis done recently, and here are the results.
PubMed Impact of Very Low Carb on CVD Risk
| Outcome | Effect Size (95% CI) | Interpretation | Number of Studies (Participants) |
| Diabetes Risk Reduction | HbA1c: -0.47% (-0.62 to -0.32) Fasting glucose: -12.5 mg/dL (-18.2 to -6.8) | Significant improvement in glycemic control, equivalent to adding a second-line medication like metformin. Reduced progression to overt diabetes in prediabetic subgroups. | 25 RCTs (1,420) |
| CVD Risk Reduction | Triglycerides: -18.2 mg/dL (-25.4 to -11.0) HDL-cholesterol: +4.1 mg/dL (+2.3 to +5.9) Systolic BP: -3.2 mmHg (-4.8 to -1.6) Framingham Risk Score: -1.8% (-2.5 to -1.1) | Favorable shifts in atherogenic lipids and BP, lowering 10-year CVD event risk by 15-20%. LDL-cholesterol was neutral overall, with no increase in particle size concerns. | 22 RCTs (1,280) |
| Endothelial Function Improvement | FMD: +1.2% (+0.7 to +1.7) Endothelial biomarkers (ICAM-1, VCAM-1, molecules that are part of the adhesive cascade in your vessels): -15% to -22% | Enhanced vasodilation and reduced adhesion molecule expression, indicating better vascular integrity and reduced inflammation. Benefits were more pronounced in those with baseline endothelial dysfunction. | 12 RCTs (680) |
What is Lipoprotein (a)?
This troublemaker is like an LDL cholesterol particle but with an added protein that makes it more prone to “sticking” to damage the vessel lining. This one should be checked due to its levels being very dominated by genetic factors. -Side note on epigenetic factors that come into play.-
What are epigenetics?
- There is growing (though still preliminary) evidence linking epigenetics and parental diets to higher lipoprotein (a). These chemical “switches” in your DNA don’t change the code but tweak how genes are expressed.
- Lp(a) is mostly genetic, but these non-genetic factors can amp up its expression across generations. Parents’ eating habits are leaving a bookmark in the epigenome that dials up Lp(a) production, raising heart risks without altering DNA.
How to reduce Lipoprotein (a)?
The greatest defense is lifestyle health. Remove high oxidative nutrition from processed garbage, epically carbs and Omega-6 fatty acids (seed oils), and use exercise benefits to help control this. Also, counterintuitively, statins raise this LP(a) by 30% in some folks. But are they are still heavily prescribed because it lowers LDL. Make sense if you don’t think about it.
Consider niacin (vitamin B3)
It has been shown to reduce Lp(a) up to 30%. It causes vasodilation, so some experience flushing of the skin. Women may want to be aware due to increase hot flash sensations. Many multivitamins contain it in the B vitamin complex. How to take it? Slow Ramp, start low (100-250mg) with food. Extended-release forms spread the hit.
What do high triglycerides mean?
Triglycerides are excess calorie “spillover” fats your liver stores from carb/sugar overload, morphing LDL into tiny, artery-penetrating missiles, warn of insulin resistance. What does this mean? There is excess glucose in your body, and the liver can’t do anything more with it. Those fats are packaged as triglycerides (the main form of stored fat) and bundled into particles called VLDL (very low-density lipoprotein). The liver then “pushes” these into the bloodstream to distribute the energy elsewhere. This raises blood triglyceride levels (hypertriglyceridemia), which is common in insulin resistance. Insulin normally binds to receptors on cell surfaces like a key in a lock, opening “doors” to let glucose in. In resistance, cells ignore the signal; insulin is still there, but the “lock” is jammed (by inflammation, excess fats, glucose). Your pancreas pumps out more insulin to compensate (hyperinsulinemia), but it eventually can’t keep up, leading to high blood sugar.
Triglyceride Study:
An August 2025 Frontiers in Nutrition meta-analysis of low-carb diets in 5,000+ patients cut triglycerides 30%, slashing CVD markers by 15% via better insulin sensitivity. January 2025 Journal of Lipid Research found that omega-3s (2g/day) drop levels by 25%, reducing events 20% in hypertriglyceridemia. Frontiers in Nutrition
Take action: Reduce carb intake and ditch alcohol.
Fasting Insulin Test: Gauging Your Cells’ Numbness to Sugar and Hidden Artery Damage
Fasting insulin measures how hard your pancreas pumps to shove sugar into resistant cells, like opening that locked door. Too much? It leads to fat spillover and vessel scarring. If you are testing this on a blood panel, you should be in a fasted state, at least 8 hours. Why? Because it shows how hard the pancreas is working to pump insulin, giving a story into early insulin resistance and metabolic syndrome. Pair with a fasting glucose to see how much sugar is in the blood. If there is a high level in a fasted state, that means there is excess sugar pumping through the bloodstream due to over consumption, even after going hours without food.
Reduce Fasting Insulin
Intermittent fasting and high-fat fat low-carb can improve this both. Resistance training builds muscle, which leads to better control of glucose in the body.
Homocysteine Levels: The Overlooked Amino Acid Damaging Arteries. And How B-Vitamins Fight Back
Homocysteine is a natural byproduct of protein breakdown in your body, but when B-vitamins (like B6, B12, and folate) are low, it builds up like rust on pipes, irritating and weakening artery walls, leading to inflammation, plaque build-up, and clotting.
B-Vitamin Fight Back:
Daily multivitamin with 400–800 mcg folate, 500-1,000 mcg B12, and 10-25 mg B6 reduces levels by 20-40% in weeks. Medications like metformin and PPIs (Proton Pump Inhibitors) deplete your B vitamins. PPIs also cause dependence via rebound reflux on days you don’t take them. A vicious cycle to keep the body needing them.
So there it is. The ultimate blood panel for heart health isn’t just a checklist
It’s your personal early-warning system against cardiovascular disease (CVD). From the plaque-spotting power of the Coronary Artery Calcium (CAC) score (catching rust before it spreads) to the inflammation alarm of hs-CRP, the particle-counting precision of ApoB (smarter than LDL alone), the sugar excess in HbA1c, the genetic wildcard of Lp(a) (sticky particle with emerging epigenetic twists), the insulin-resistance flag in Fasting Insulin and Total Triglycerides, and the overlooked artery-etcher Homocysteine (tamed by B-vitamins). These 8 tests paint the full picture of atherosclerosis, from oxidation cascades and macrophage mayhem to clot risks and metabolic memory.
These biomarkers dominate over basic cholesterol checks
Spotting 30–50% more hidden threats per 2025 meta-analyses across The Lancet and JACC. Optimal levels are achievable with targeted tweaks like low-carb swaps, omega-3 boosts, niacin for Lp(a) nudges, and folate for homocysteine. The payoff? Up to 80% slashed CVD risk, longer vitality, and peace of mind that you’re steering, not reacting.
We aren’t powerless in this battle. Knowledge is the antidote. Armed with this guide, you’re steps ahead of the curve, ready to decode your numbers and flip the script on silent plaque-builders.
Blood Panel Review:
Take ownership of health. Interested in an audit of your most recent blood panel? Shoot us an email for a free 15-minute review of the biomarkers on your panel. Gain insight into how to order a more in-depth panel, leading to a better understanding of health.
Not medical advice. Always consult with your medical professional team.