Inflammation’s Role
Inflammation is a bodily response needed in the cascade of events that is healing. Often, it is viewed as negative, and we should combat it at every turn.
This intrinsically beneficial mechanism aids our physiologic outcomes via the removal of offending substrates and restoring valuable tissue. It is the mechanism needed in the rebuilding process of our bodies.
Response in The Body
A simple way to describe it: our own internal firefighter. We wouldn’t want to stop them from going out all the time, would we?
Alternatively, we don’t want to hear those sirens going 24/7. That would be outright unreasonable. Well, our body agrees.
From this, we may anticipate that chronic inflammation can connect the incidences of arthritis, asthma, and tissue damage. Also predisposing the avenue for autoimmunity, skin breakouts, and hormone disruption in our bodies.
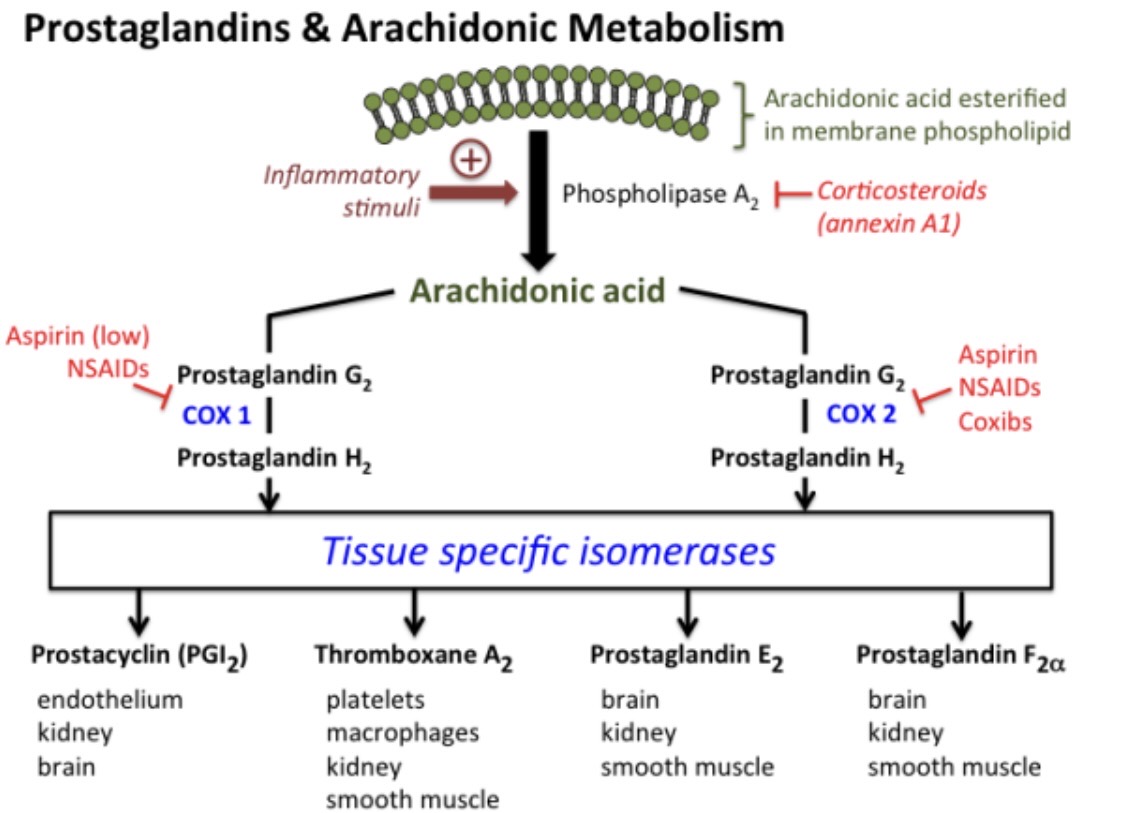
Let’s look at the inflammation cascade.
When something occurs outside our body and causes harm inside our body response. Broadly, here are the steps.
First cytokines (like IL-6) respond and sound the alarm in the whole body (systemically).
Then the crew takes action at the point of friction, so where the affected cells are.
They receive a call from the cytokines to activate cycloxygenase (the enzyme that NSAIDs shut down), which then sets the action in motion.
Starting with Arachidonic Acid from the cell membrane. Cox enzymes convert Arachidonic acid (AA) into prostaglandins. Alongside, thromboxane a2 (TXA2) follows. TXA2, a very powerful lipid mediator, promotes blood clotting (coagulation) by causing platelets to clump together (aggregate) and by constricting blood vessels (vasoconstriction). It is crucial in the homeostasis of proper clotting, and without it, we would bleed to death. Although having excess brings increase risk of stroke and cardiac events.
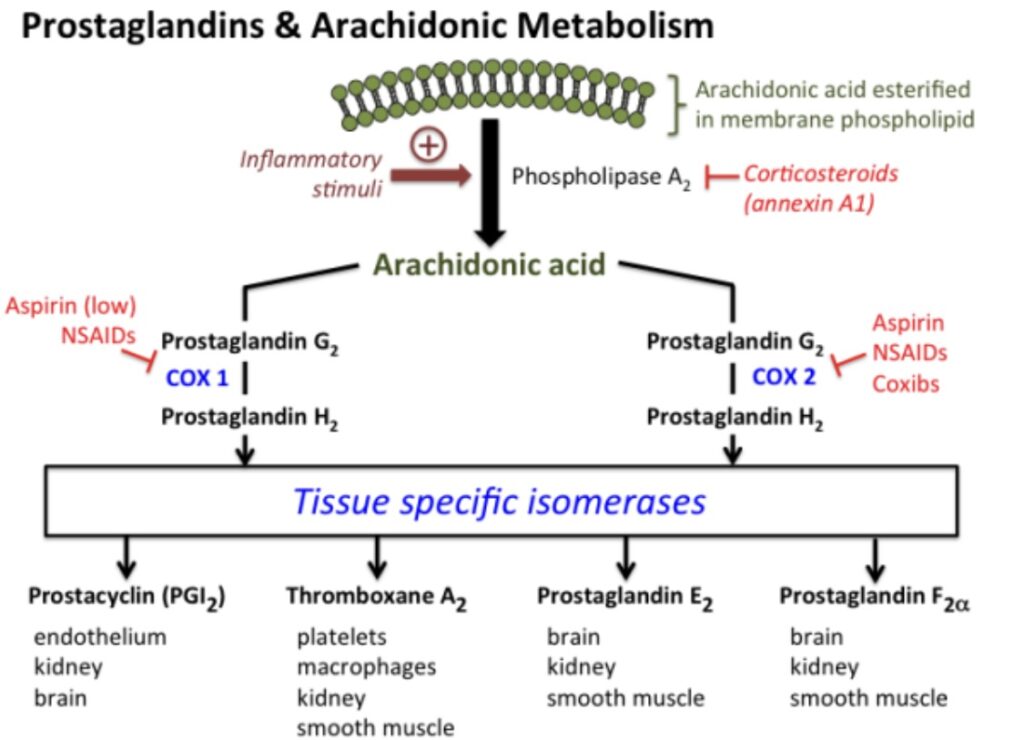
When looking at prostaglandins, of note, PGE2 is the primary mediator and is commonly attributed to a more aggressive inflammation response.
The acute phase continues with an influx of granulocytes, neutrophils, and then monocytes that mature into macrophages. They then engulf old or damaged cells. We call this phagotycocis. Once the clean-up crew is done engulfing the damaged substrate, they move out.
The prostaglandins also tell the cells in the area to become more permeable, allowing for more blood flow and therefore nutrients to the area. This causes edema, or swelling, and redness, due to the vasodilation of vessels.
From this, we typically see the objective signs of rubor (redness), calor (heat), tumor (swelling), and dolor (pain), commonly associated with injury and the inflammation response.
From this understanding, we can look at the mechanism that assists in the production of prostaglandins. Specifically, Omega-6 fatty acids. the precoursor to arachidonic acid, a building block of prostaglandins.
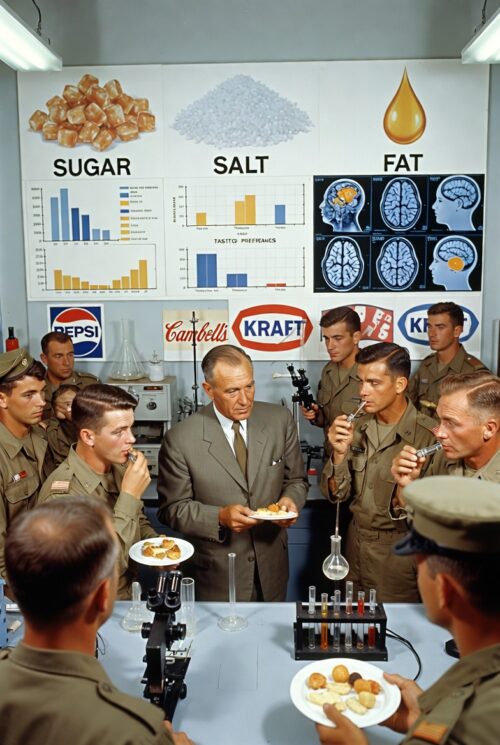
Although Omega-6 is needed in the cell membrane to prevent rigidity. We find an issue with the abundance of omega-6 fatty acids, specifically in our diet. Primarily from industrially processed seed oils.
The ratio of omega-6 to omega-3 should be around 4:1 or less. In the typical diet, we see a ratio of up to 20:1, omega-6 dominant.
This results in an excess of AA in the cell. Therefore, causing a permeable and bloated membrane to the extent that it is problematic.
To add insult to injury. When the cells have excess AA, they are overproducing PGE2, the more problematic enzyme to have in constant production.
This fuels dysbiosis, autoimmunity, pro-allergenic, and pro-thrombotic states.
Rheumatoid arthritis (RA) is a chronic autoimmune disease where the immune system attacks the joint linings, causing painful inflammation.
Studies show omega-3 fatty acids (like EPA and DHA from fish oil) can help ease RA symptoms, as a meta-analysis of 17 trials confirmed benefits for RA, inflammatory bowel disease, and menstrual pain.
Cutting arachidonic acid intake to under 90 mg/day reduces RA inflammation, and adding fish oil amplifies those effects even more. At least 11 double-blind trials back fish oil for RA, including less need for pain meds, by helping immune cells stay non-inflammatory and reset chronic ones to normal.
Omega-3s (EPA/DHA from fish oil), pack into cell membranes, crowding out AA (from seed oils). This shifts the balance: More EPA means less AA available as raw material.
In Crohn’s patients, there is increased COX-2 expression in colonic epithelium. Therefore, the inflamed colon produces excess prostaglandins. Oxidized linoleic acid heightens oxidative stress and triggers IL-8 (an inflammation signal) in these cells. The findings lead researchers to recommend cutting dietary linoleic acid and adding antioxidants to ease symptoms.
Current overconsumption of omega-6 acid may lead to a hyperallergenic state, being causal of asthma and increased risk of eczema. Longer trials are needed to conclude if omega-3 provides benefits for asthma, but omega-3 supplementation has shown a lower asthma severity score than the omega-6 cohorts.
Much of the population is disproportionately deficient in omega-3 fatty acids. It would be beneficial to educate on the importance of understanding that inflammation is not the enemy in our bodies. Managing with dietary interventions has been shown to be advantageous.
Foods high in omega-3 content are fatty fish like salmon, mackerel, and sardines. Walnuts are a viable source, and grass-fed beef has a higher omega-3 to omega-6 ratio, compared to grain-fed sources, where the corn/soy feed overloads the AA precursor.
Cardiovascular disease (CVD) ranks as the world’s leading cause of death. Thrombosis serves as the primary driver behind the three largest CVD threats:
-ischemic heart disease
-ischemic stroke
-venous thromboembolism (VTE).
Omega-3 and omega-6 polyunsaturated fatty acids are key building blocks in platelet membranes, helping control how platelets clump and form clots.
Adding more of these fats through diet can reshape platelet membranes and tweak their activity, potentially slowing heart disease and cutting clot risks. Understanding how these fats and their byproducts influence platelets could unlock new treatments for blood clotting issues.
The overabundance of AA, therefore, PGE2, and TXA2 may then play a role in the increased prevalence of atherosclerosis in the population, giving weight to the oversimplified resolution of lower LDL cholesterol.
In conclusion, our diets have an overabundance of a needed fatty acid. Having most anything in excess typically brings an unfavorable result. The simplest mechanism for change would be to understand that the abundance of processed food is not advantageous to any measure of health.
Much of the population is deficient in omega-3 and could potentially see benefit from adding more into the diet. With consideration of the source (i.e., quality supplementation, not oxidized cheap forms) and concentrations of mercury content in marine food sources.
Inflammation is a beneficial action in the chain of healing and should be welcomed in the acute phases of injury. When chronic pain prevails, underlying lifestyle factors should be examined. And measures should be taken to improve the abundance of pro-inflammatory substrates.
Send an email to info@solutions2welllness.org for a in-depth look into health and nutrition